Sepsis may start with a high-grade fever, difficulty breathing, or an accelerated heart rate and can quickly become more severe. When left untreated, the illness can progress to severe sepsis, where the organs, including the kidneys and heart, are affected. The final stage of sepsis is septic shock. Victims of nursing home neglect have a greater risk of death and severe disability from sepsis.
Sepsis is a life-threatening condition that causes your immune system to go into overdrive as it tries to battle an infection. Sepsis has three stages, and the earlier the condition is caught, the better chance for survival. People suffering from nursing home neglect may reach the third stage before being brought in for treatment.
According to the CDC, “the sepsis-related death rate among adults aged 65 and over was 277.4 per 100,000.” Death rates for those aged 85 and older were five times higher than adults aged 65 to 84, making it a serious and often fatal condition for the age group that comprises the largest percentage of nursing home residents.
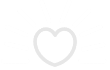
Stage One: Sepsis
The first stage of sepsis is the easiest to treat but sometimes difficult to detect, especially early on. Diagnosis is difficult because the early symptoms resemble many other common illnesses, such as respiratory infections and viruses.
A change in body temperature often marks the early stage of sepsis. For some patients, a high fever is common, ranging around 101 degrees Fahrenheit or higher. In others, they will have a lower body temperature, often running around 96.8 degrees Fahrenheit.
Other signs of the first stage of sepsis include:
- An accelerated heart rate. Usually higher than 90 beats per minute
- An infection that blood culture tests have confirmed
- A breath rate of 20 per minute or higher
A doctor must confirm these symptoms, and two or more symptoms must be present before sepsis is suspected. Catching sepsis in this early stage can significantly improve the chances of survival as it is likely to have not affected any vital organs at this point.
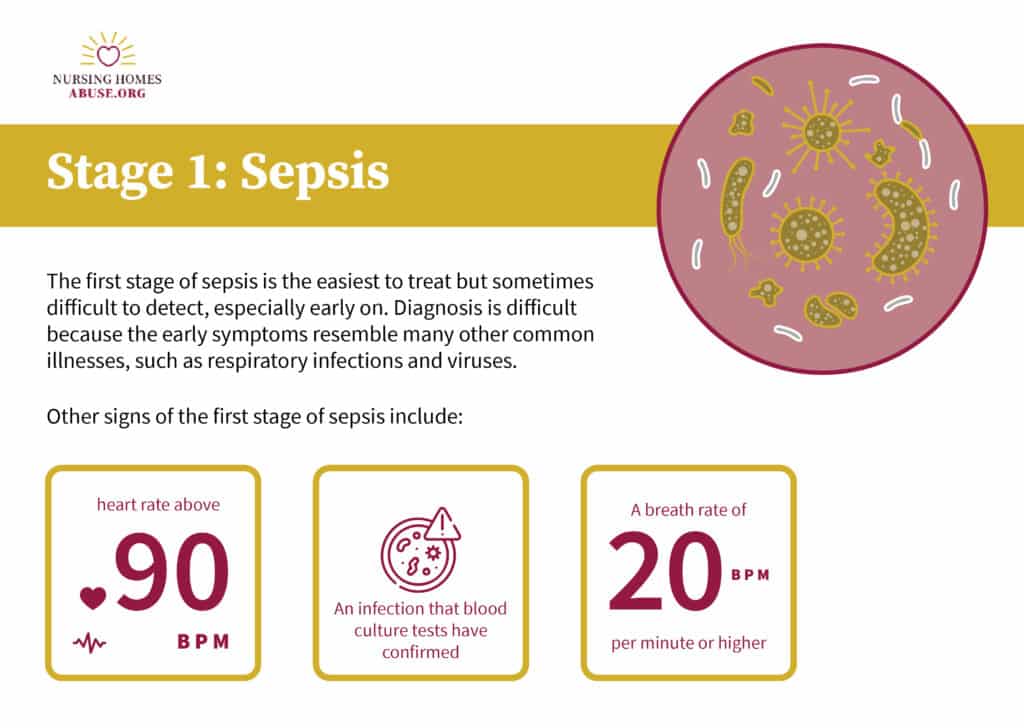
Stage Two: Severe Sepsis
If the sepsis is not detected or is resistant to the initial treatment in the first stage, it will progress to the second stage, known as severe sepsis, according to MedlinePlus. At this stage, the possible complications are more serious as the condition will begin to affect the function of vital organs.
The presence of two to three symptoms is required for a severe sepsis diagnosis. A decrease in urination is one common sign of severe sepsis. Decreased urination occurs as sepsis begins to affect the function of the kidneys.
If the sepsis affects the heart or circulatory system, the patient may develop abnormal heart functions or chills from trouble maintaining their body temperature.
Other severe symptoms may accompany this stage of sepsis, including:
- Changes in mental processing or ability
- A lower than normal platelet count, which means reduced blood clotting ability
- Rapid breathing or difficulty taking deep breaths
- Discolored patches underneath the skin
- Extreme weakness throughout the extremities
- Bluish coloring around the extremities and lips
- Loss of consciousness
While these symptoms are severe on their own, without immediate medical attention, the situation can become deadly rapidly. If you have a loved one with any of these symptoms and suspect severe sepsis, they could be a victim of nursing home neglect.
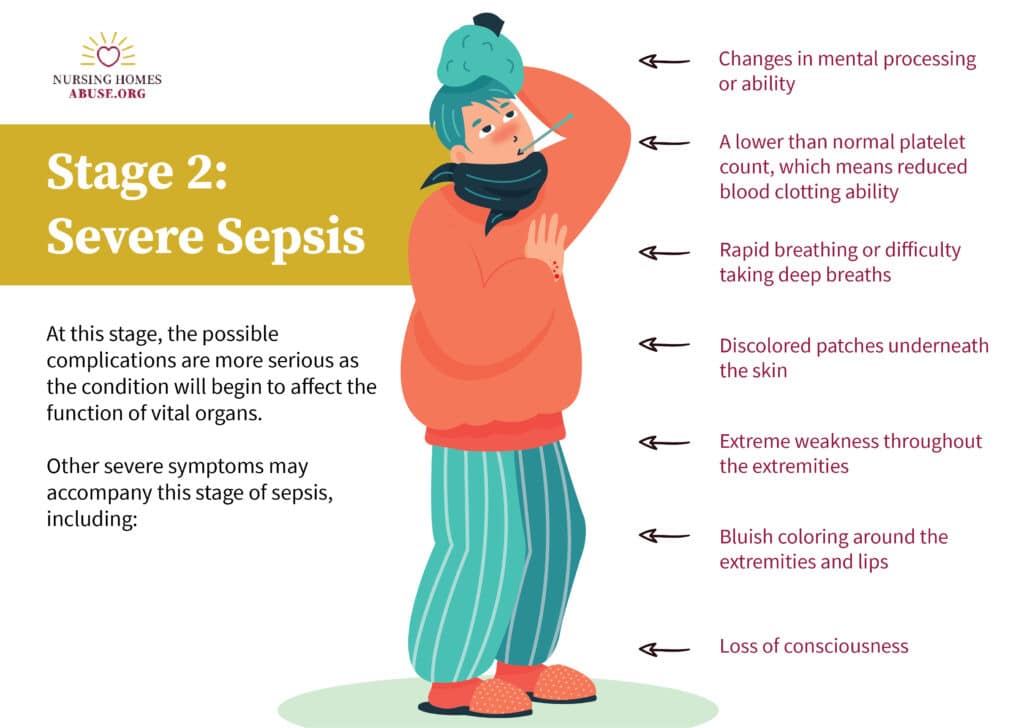
Stage Three: Septic Shock
Once your loved one reaches the final stage of sepsis, they have reached septic shock, which puts them in a medically dangerous situation. Symptoms of septic shock are similar to the symptoms of the first two stages, but they are more pronounced. In addition to these symptoms, Mayo Clinic notes, there is a significant drop in blood pressure.
The drop in blood pressure is one of the symptoms that can turn sepsis deadly. These drops can result in:
- Stroke
- organ failure
- respiratory failure
- heart failure
- immediate death
During septic shock, medical intervention can sometimes not affect dropping blood pressure. Elevated lactate levels will increase as the body continues under stress.
A 2020 study published in Critical Care noted a 90-day septic shock mortality rate of 38.5%, as revealed by a systematic review of 170 articles from PubMed and the Cochrane Database between 2009 and 2019.
What is post-sepsis syndrome?
Those who survive sepsis may not always return to pre-sepsis health. In some cases, there can be lasting consequences that take the form of post-sepsis syndrome.
This condition most commonly occurs in patients who spent time in the intensive care unit for their sepsis or those with an extended hospital stay. These symptoms vary in severity and may be experienced for a while after sepsis recovery or permanently.
According to Sepsis Alliance, post-sepsis syndrome often includes disturbances to regular sleep, which can lead to debilitating fatigue during the day.
Persistent rashes and hair loss can also occur with post-sepsis syndrome, along with painful joints and a lack of appetite.
Some symptoms are more severe and can have long-term health consequences including renal failure and cardiovascular events. Breathing can also remain difficult after recovering from sepsis which can exacerbate fatigue and cardiovascular problems.
Aside from physical symptoms, those with post-sepsis syndrome may also experience emotional and cognitive impairments. These patients may experience vivid nightmares, recurring panic attacks, and depression due to their ongoing health concerns.
In many cases, severe post-sepsis syndrome will result in re-hospitalization and a diminished quality of life.
Any type of infection in the body can result in sepsis, with the most common being infections of the bloodstream, kidneys, and abdomen or pneumonia.
Unfortunately for those in nursing home facilities, a lack of proper health monitoring may lead to a rapid progression through the three stages, resulting in severe disability or death.