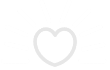
Bedsores, also known as pressure ulcers, are skin wounds caused by prolonged pressure on the skin. People with limited mobility are at the highest risk of developing bedsores because they spend long hours sitting or sleeping in the same position. With time, the skin experiencing the most pressure suffers from a lack of blood supply and develops a wound.
Bedsores affect more than 2.5 million people in the United States every year. There are multiple stages of bedsores based on the severity and depth of the wound. Stage 1 sores can heal within three days. Stage 4 bedsores are the most serious and heal within a few months when treated properly. However, a lack of appropriate treatment can result in other complications, such as infections, which can make the situation worse.
Stage 1 Bedsores
Stage 1 bedsores only affect the upper layer of the skin. The patient may complain about mild pain in the area or have a visible change in skin appearance.
Symptoms
The main signs and symptoms of stage 1 bedsores include:
- Mild discoloration: skin that appears reddish, bruised, or darkened
- Swollen skin
- Skin that is painful to touch
- Skin that feels warmer than the other parts of the skin
What to Do
A stage 1 bedsore is caused by too much pressure on the area. Any additional pressure on the ulcer can worsen the condition, so the first treatment step is to alleviate the weight or compression. If a patient has limited mobility, a caregiver can turn or adjust them to provide relief.
Ensure that the ulcer is clean and dry. You can clean it with warm water and mild soap to remove any germs on the surface, which could cause an infection.
Some foods, including those rich in protein, zinc, and iron, can facilitate healing. Drinking plenty of water can also help as it keeps the body hydrated and makes the skin firmer.
Recovery
When treated early, stage 1 bedsores can heal within three days. However, you should reach out to your doctor for further treatment if the ulcer persists for more than three days.
Stage 2 Bedsores
Stage 2 bedsores happen when stage 1 bedsores worsen. The sores appear larger and are more painful.
Symptoms
In the case of a stage 2 bedsore:
- The upper skin layer might be broken, creating a small wound.
- The affected skin may be swollen and very painful.
- The surrounding areas may have small blisters and might appear darker.
- There could be pus or drainage, signifying an infection.
What to Do
Change the sleeping or sitting position of a bedridden patient immediately to prevent the ulcer from becoming worse. Also, ensure that the wound is clean. Stage 2 bedsores require more careful handling because the skin is sensitive, so seek a doctor’s guidance in cleaning your wounds.
A caregiver may consider giving the patient some pain relievers when cleaning the wound. Additionally, ensure that the patient follows a balanced diet and drinks lots of water. Lastly, seek a doctor’s help if the wound releases pus or develops more blisters. Any form of drainage or bad odor from the affected area signifies infection, and you’ll need a doctor to help you treat it.
Recovery
It takes a minimum of three days and a maximum of two weeks to recover from a stage 2 bedsore. Be sure to call a doctor if the wound takes longer to heal.
Stage 3 Bedsores
Stage 3 bedsores are even deeper and more extensive than stage 2 sores. At this stage, the wound has damaged the top two layers of skin and affected the layer of fatty tissue just beneath the skin. The resulting wound is crater-like, and more prone to infections because of the exposure of the fatty layer.
Stage 3 bedsores happen when the blood supply is completely cut off to the area. The result is that the healthy tissue in that region is damaged, creating an open wound.
The main risk factors for stage 3 bedsores are diabetes, spinal injuries resulting in limited mobility, malnutrition, and blood circulation issues.
Symptoms
The following symptoms can signify stage 3 bedsores:
- Bad odor
- Black skin surrounding the wound
- Redness and possible swelling
- Greenish drainage and pus
- Fever
What to Do
Stage 3 bedsores are severe and need the attention of a doctor who will carefully examine the wound, clean it, and apply the proper medications. However, first, reduce the pressure on the area by making the patient more mobile or turning them to rest and sleep in other positions.
If possible, provide the patient with a special cushion or mattress to increase their comfort. Depending on the severity of the condition, the doctor may provide antibiotics to treat the infection and then remove any dead tissue from the wound.
Recovery
Stage 3 ulcers can take up to four months to completely heal. Patients with bedsores at this stage may require additional treatment if the recovery process takes longer.
Stage 4 Bedsores
Stage 4 bedsores result in the most complicated wounds. These ulcers occur when stage 3 wounds are not treated properly. The sores are large, affecting the fatty tissues, bones, muscles, and ligaments. Patients with stage 4 bedsores experience severe pain, and their movement may be limited.
Symptoms
Symptoms of a stage 4 bedsore can be extremely severe, including:
- A deep and extensive wound that exposes the bones and ligaments
- Pus and drainage signifying an infection in the wound
- Swelling and blisters around the wound
- Darkened skin that is extremely sensitive
- High fever, in some instances
What to Do
Stage 4 bedsores should be treated immediately. The first step is to reduce the pressure on the wound. Ensure that the patient does not wear tight clothes or rest on the affected area.
A doctor should clean the wound because of the severity of the condition. After cleaning, the doctor will likely recommend antibiotics to kill any bacterial infections.
Other treatments for stage 4 bedsores include:
- Skin grafts: A doctor may surgically cover the affected area with healthy skin.
- Debridement: This is a procedure in which a doctor removes dead or infected tissue from the wound, to help it heal.
People with stage 4 bedsores require close monitoring. It’s essential to listen to the patient’s complaints and take the proper actions. Examine the condition of the wound every day and report any changes. In addition, ensure that the patient gets a balanced diet and drinks enough water.
Recovery
Recovery from a stage 4 bedsore depends on how soon treatment starts and its effectiveness. While some wounds can heal in three months, others can persist for years. The key is to ensure that you or your loved one starts treatment immediately after noticing the wound.
Unstageable Bedsores
Unstageable bedsores are wounds whose severity cannot be determined unless a doctor cleans them first. These wounds may be covered by slough or eschar, which are two different types of dead tissue that can be present in open wounds. Eschar is thick and dry, while slough is moist and stringy. A doctor will need to remove any slough or eschar to examine the sore properly and determine how deep it is.
Symptoms
In the case of an unstageable bedsore:
- The wound may appear reddish or greenish if there is an infection.
- The patient may have severe pain and swelling.
- The patient may have a fever.
What to Do
Only an experienced doctor should handle unstageable bedsores. The doctor should clean and diagnose the wound to know its stage and recommend further treatment.
Deep Tissue Injuries
Like unstageable bedsores, deep tissue injuries can be hard to detect. The wound on the upper part of the skin looks like a stage 1 or stage 2 bedsore. However, below the surface, it might be stage 3 or 4. With deep tissue injuries, a thin blister can form on the skin, covering the wound and making it difficult to diagnose its exact stage.
Symptoms
If you suspect a deep tissue injury, watch for:
- Localized skin discolorations
- A wound that is warmer or cooler than surrounding skin
- Severe pain and high fever
Note that any skin discoloration may be harder to see on darker skin
What to Do
Frequently reposition the patient to reduce excess pressure on the wound. Ensure the skin is dry, and avoid covering it with tight clothes. Keep the bedsheets dry and pay attention to the patient’s complaints.
An experienced doctor should do an ultrasound in order to understand the depth of the wound. They will then recommend treatment.
How To Prevent Bedsores
The following measures can help you or your loved one prevent bedsores:
1. Prevent Direct Pressure
Direct pressure is the primary cause of bedsores. It interrupts blood flow to the skin, which creates a wound.
Avoid excessive pressure by using comfortable mattresses and cushions. A bedbound person should also frequently change the position of their body. Ideally, they should change position at least every 2 hours and every 30 minutes for someone who is especially susceptible to bedsores.
2. Provide the Right Skincare
Ensure that skin is clean and dry at all times. Use mild soap, water, and moisturize the skin well after cleaning. Those with sensitive skin can ask a doctor for product recommendations.
3. Eat a Balanced Diet
A balanced diet prevents malnutrition, which puts an individual at risk for bedsores. Be sure to eat plenty of protein, minerals, and vitamins. In addition, be sure that you’re getting enough water to stay hydrated. For most healthy people, the recommendation is to drink at least two liters of water every day. For those with certain health conditions, such as kidney problems, it’s possible to drink too much water, so consult with your doctor for specific recommendations.
4. Maintain Hygiene
Sleeping or resting on a clean surface at all times helps protect skin. Bed sheets should always be clean and dry. Cotton is an excellent choice of material because it reduces friction.
5. Manage Chronic Health Conditions
Chronic health conditions such as diabetes interfere with the blood supply in the body and increase the risk of bedsores. If you or your loved one has heart disease, kidney problems, or any other chronic conditions, be sure to maintain a healthy diet, take any prescribed medications, and follow the doctor’s advice to reduce the risk of bedsores.
6. Tell A Doctor About Skin Changes Or Discomfort
Do not ignore the mild changes in you or your loved one’s body or skin. They may indicate a more significant problem. If anything seems wrong, consult a doctor.
Possible Complications of Pressure Sores
Without proper treatment, bedsores can result in multiple complications. Here are some of the issues that can develop:
Cellulitis
Cellulitis is a bacterial infection of the skin. The infection may spread into deeper layers of tissue and cause complications. If the bacteria spread into the bloodstream, this can be a life-threatening situation. Patients who have untreated open wounds for long periods are the most susceptible to cellulitis.
Bone or Joint Infections
Prolonged bedsores can result in bone or joint infections. These infections can reduce the functionality of the affected bones and joints.
Cancer
Wounds that go untreated for an extended period and cannot heal can increase the chances of developing cancer cells.
Mental and Financial Complications
Like other illnesses, bedsores can affect a patient’s mental health and drain their financial resources. This is especially true when a wound lasts for many years.
When should I see a doctor?
Call a doctor immediately if you notice any of the following symptoms in yourself or a loved one:
- Signs of infection: drainage, bad odor, change in color, swelling, or increased redness
- Blisters around the wound
- High fever
The doctor should closely examine the wound and apply medication. If the condition is extreme, they may schedule surgery.
Bedsores in Nursing Homes
Anyone can get bedsores, but the elderly population is the most vulnerable. If you have a loved one in a nursing home, ensure that they receive the best care possible to avoid neglect and further injury. Monitor their health and pay attention to their complaints. If they develop bedsores, help them get the proper medical services.
In addition, do not hesitate to seek legal help for bedsores resulting from nursing home abandonment. You may be able to receive compensation for any suffering. Request a free case review today.